Studies Archive
Rate of Telehealth Decline from 2020 to 2021 Inconsistent Across States
December 12, 2021Last week, HHS’s Office of the Assistant Secretary for Planning and Evaluation (ASPE) released a report analyzing Traditional Medicare Part B telehealth utilization in 2020. The study outlines that while in-person Medicare visits decreased in 2020 compared to 2019, telehealth visits increased 63X to 52.7M visits. However, the volume increase was not sufficient to offset the loss of in-person care. Notably, 28.3M, or 53%, of Medicare beneficiaries (inclusive of Traditional and Medicare Advantage) utilized telehealth in 2020.
At the outset, it is noteworthy that the comparison of 2019 to 2020 is anything but an “apples to apples” comparison. Most notably, the very definition of telehealth changed in the comparison period, with two-way interactive video conversations being a required component of a reimbursable “telehealth visit” in 2019, whereas “audio-only” encounters and virtual check-ins, previously components of visits, were considered independent telehealth visits in 2020. The report notes that the Centers for Medicare and Medicaid Services (CMS) classified telehealth visits broadly to account for the types of services added and allowed for the duration of the public health emergency. Notably, codes for virtual check-ins were only introduced in 2019 by CMS, but do not meet the statutory definition of an interactive telehealth visit.
In spite of the broad expansion of the definition of a “telehealth visit” as a result of the pandemic, telehealth utilization for traditional medical services is nominal. Of Medicare Part B visits, just 2% of specialty visits and 8% of primary care visits in 2020 were delivered via telehealth, compared to over 38% of behavioral health visits. This reinforces our prior research challenging telehealth’s viability as a substitute good for a broad range of services, rather than a subset of services (e.g., behavioral health).
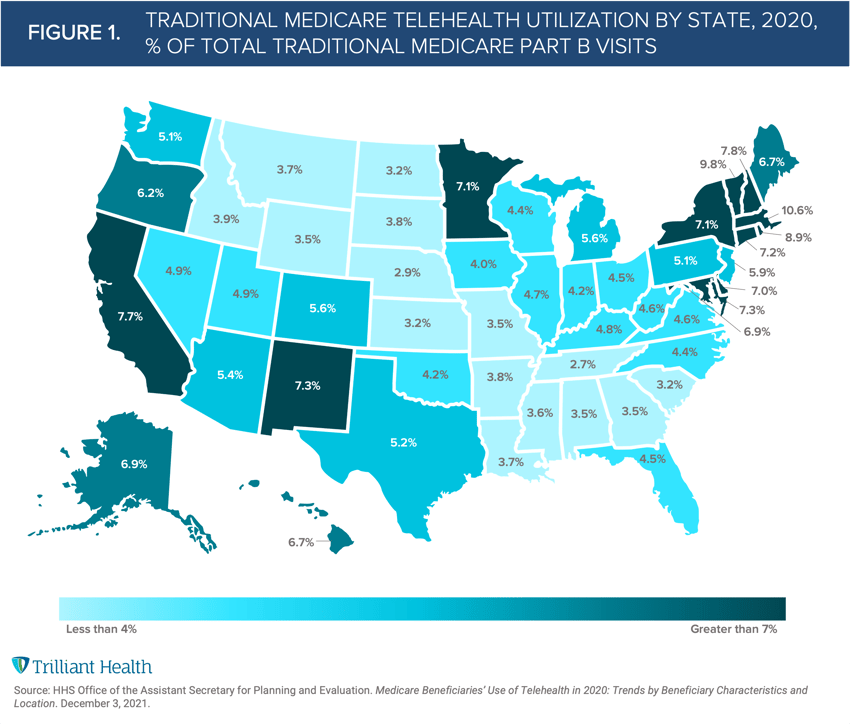
Further reinforcing our findings, the ASPE study also highlights how telehealth utilization varied geographically. Regionally, Massachusetts (10.6%), Vermont (9.8%), Rhode Island (8.9%), New Hampshire (7.8%), and Connecticut (7.2%) had the highest 2020 telehealth utilization (as a percent of all Part B visits), while Tennessee (2.7%), Nebraska (2.9%), Kansas (3.2%), North Dakota (3.2%) and Wyoming (3.5%) saw the lowest utilization (Figure 1). Although CMS temporarily relaxed several Medicare telehealth coverage restrictions, not all beneficiaries have the same level of access to or desire to use telehealth. For example, beneficiaries with limited broadband access cannot feasibly access synchronous audio-video services.
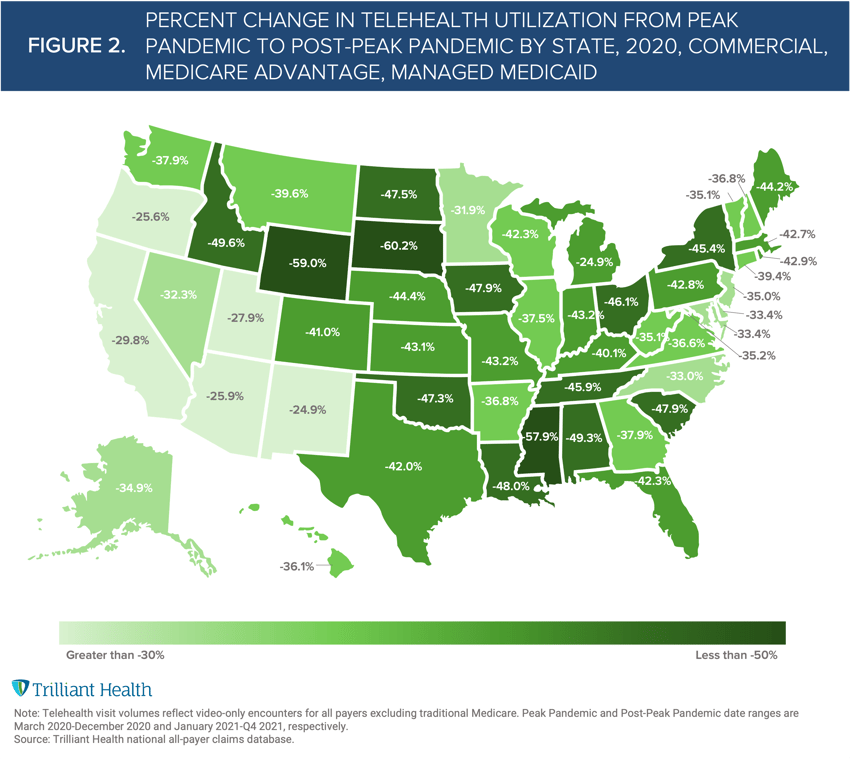
The ASPE analysis provides a holistic picture 2020 Traditional Medicare telehealth utilization, offering the final piece needed to evaluate pandemic-era telehealth utilization across coverage types. To compare across coverage sources, we analyzed how average monthly telehealth utilization has changed by state from the peak pandemic (March - December 2020) compared to this year using our all-payer claims data (excluding Traditional Medicare).
Telehealth utilization has dropped across all states compared to 2020, averaging a 40.3% decline in monthly visits (Figure 2). In states with the highest Traditional Medicare telehealth visits, as a proportion Part B visits, telehealth utilization declined, on average, as follows:
-
Massachusetts: -42.7%
-
Vermont: -35.1%
-
Rhode Island: -42.9%
-
New Hampshire: -36.8%
-
Connecticut: -39.4%
Whereas the utilization changes in states with the lowest Traditional Medicare telehealth visits are:
-
Tennessee: -45.9%
-
Nebraska: -36.8%
-
Kansas: -43.1%
-
North Dakota: -47.5%
-
Wyoming: -59.0%
While these trends are derived from different coverage sources than Traditional Medicare, utilization patterns at the state level are driven by more than coverage source, and thus are useful in understanding where utilization has changed in 2021.
ASPE’s analysis addresses several questions regarding Medicare telehealth utilization, which will inform the potential permanence of relaxed Medicare coverage restrictions. However, the report also raises several new questions, particularly around 2021 Medicare telehealth utilization and which of the 53% of Medicare beneficiaries are still using telehealth. Understanding regional and local telehealth trends will better inform federal policy change and pose the question of what the local drivers of regional utilization are.
Thanks to Kelly Boyce and Katie Patton for their research support.
- Virtual Care
- Medicare & Medicaid






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)



