The Compass
Sanjula Jain, Ph.D. | September 18, 2022The Secular Decline in Average Age of Surgical Patients Aligns with Recent Trends in Life Expectancy and Excess Mortality
Key Takeaways
-
In just two years of the COVID-19 pandemic, U.S. life expectancy declined 2.7 years, from 78.8 in 2019 to 76.1 in 2021, a trend that is compounded by growing excess mortality particularly in younger adult cohorts (ages 25-45).
-
Although the median age in the U.S. and number of Medicare beneficiaries continues to increase, the average age of surgical patients has declined sequentially since 2018.
-
The average age of orthopedic surgery patients declined 4.2 years, on average, between 2018 and 2021, while the average age of lung surgery patients declined by 1.6 years.
COVID-19 has exacerbated pre-pandemic declines in average U.S. life expectancy and excess mortality of younger age cohorts.1,2 The implications of these shifts in population demographics on the health status of, and utilization of healthcare services by, the U.S. patient population will be significant.
Background
Average U.S. life expectancy has declined since 2015, peaking at 78.9 in 2014 after steadily increasing for decades (Figure 1). In just two years of the COVID-19 pandemic, U.S. life expectancy declined 2.7 years from 78.8 in 2019 to 76.1 in 2021, the lowest it has been since 1996. The CDC has concluded that between 2020 and 2021, the top three contributors to declining life expectancy were COVID-19 (-50%), unintentional injuries such as drug overdoses (-15.9%), and heart disease (-4.1%).3
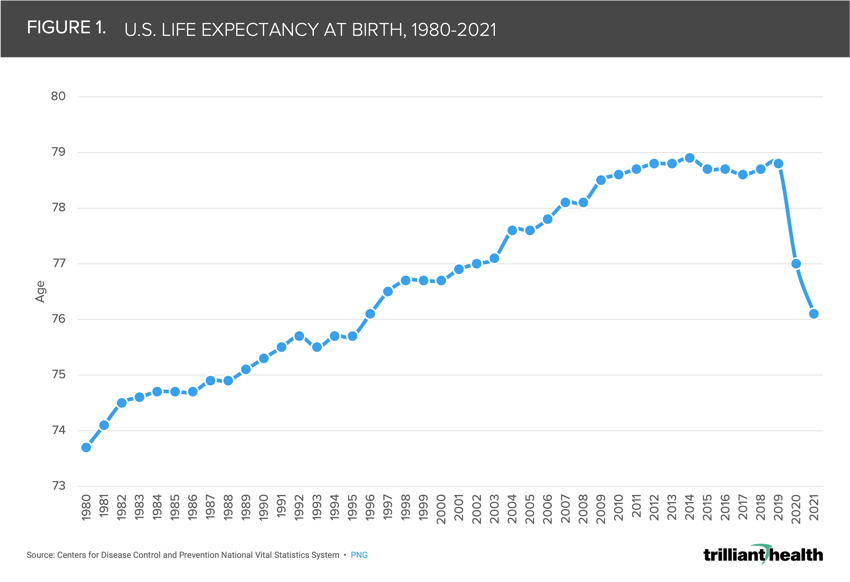 Moreover, the magnitude of declining life expectancy is further compounded by growing excess mortality. Evidence of this phenomenon is particularly notable in a younger adult cohort (ages 25-45), which experienced a disproportionately large share of COVID-related and non-COVID-related excess mortality since the pandemic’s onset.4
Moreover, the magnitude of declining life expectancy is further compounded by growing excess mortality. Evidence of this phenomenon is particularly notable in a younger adult cohort (ages 25-45), which experienced a disproportionately large share of COVID-related and non-COVID-related excess mortality since the pandemic’s onset.4
Historically, there were two certainties about the U.S. healthcare delivery system: commercially insured patients generated higher operating margins than other patients, and Medicare beneficiaries utilized more healthcare services than other patients. A permanent decline in the healthcare utilization of both commercially insured patients and Medicare beneficiaries would impact every health economy stakeholder and would be particularly detrimental for hospitals, whose high capital and operating costs require an increasing volume of patients to create incremental operating margin at the unit level.
Analytic Approach
To identify trends in average patient age, we focused on the annual average surgical patient age as an indicator of intensity of care. We analyzed data from patients across all pay types (Medicare, Medicaid, and commercial) from 2018 to 2021 for orthopedic, cardiac, lung, and cancer surgeries.
Findings
Although the median age in the U.S. and Medicare enrollment continues to increase, the average age of surgical patients across pay types, both in the inpatient and outpatient settings, has sequentially declined since 2018 across all service lines included in the analysis.5,6 The average orthopedic surgery patient age declined most (-7%) between 2018 and 2021, dropping 4.2 years on average, while lung surgery patient age declined least (-2.4%) in the same time period, dropping only 1.6 years on average.
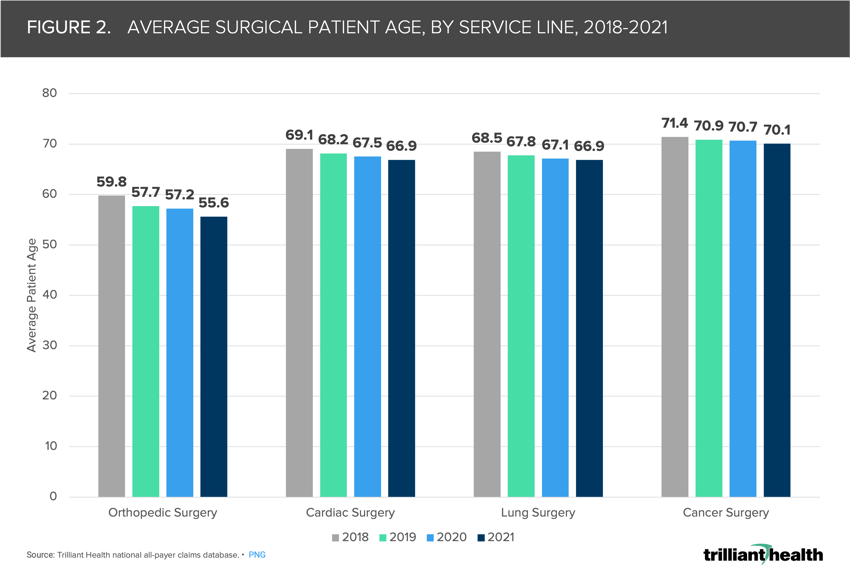 Sustained excess mortality of younger age cohorts and the stark two-year decrease in average U.S. life expectancy partially “explain” this observed decrease in average surgical patient age. If younger individuals, on average, have been receiving more intensive care (e.g., surgery) before and after the pandemic, thus bringing down average patient age, it is necessary to identify which interventions are necessary to address worsening patient acuity and increased mortality risk for younger patients.
Sustained excess mortality of younger age cohorts and the stark two-year decrease in average U.S. life expectancy partially “explain” this observed decrease in average surgical patient age. If younger individuals, on average, have been receiving more intensive care (e.g., surgery) before and after the pandemic, thus bringing down average patient age, it is necessary to identify which interventions are necessary to address worsening patient acuity and increased mortality risk for younger patients.
Importantly, given these trends continue to parallel overall declining patient volumes, health economy stakeholders will be further challenged to optimize patient yield in an economy with a lower number of patients overall, many of whom are demonstrating a low propensity to return to care.7,8 With healthcare affordability an increasing concern for most Americans, the barriers to re-engaging patients in necessary medical care will be even greater.
Thanks to Kelly Boyce and Katie Patton for their research support.
- Disease Burden
You are currently viewing a free preview of our premium studies. To receive new studies weekly, upgrade to Compass+ Professional.
Sign UpSee more with Compass+
You are currently viewing the free version of this study. To access the full study, subscribe to Compass+ Professional for $199 per year.
Sign Up for Compass+