Research
Match Day 2024: Primary Care Residency Positions Continue to Go Unfilled
Apr 7, 2024 12:01:00 AMKey Takeaways
-
During the 2024 Residency Match cycle, 80.2% of students with a certified rank order of training preferences matched to a first-year residency position, while the total number of available positions increased by 2.8% compared to 2023.
-
Primary care specialties had the highest number of unfilled residency positions: family medicine (1,272 unfilled positions), internal medicine (988 unfilled positions) and pediatrics (502 unfilled positions).
-
In contrast to primary care, most specialist residency positions (e.g., surgery, anesthesiology and otolaryngology) were 100% filled.
- The specialties among the lowest projected adequacy rates for 2036 are internal medicine (75.8% adequate) and family medicine (78.3% adequate), while specialties with the highest adequacy rates are emergency medicine (122.9% adequate) and endocrinologists (109.6% adequate).
- Across primary care physician specialties, adequacy projections are consistently lower in rural areas than in non-rural areas.
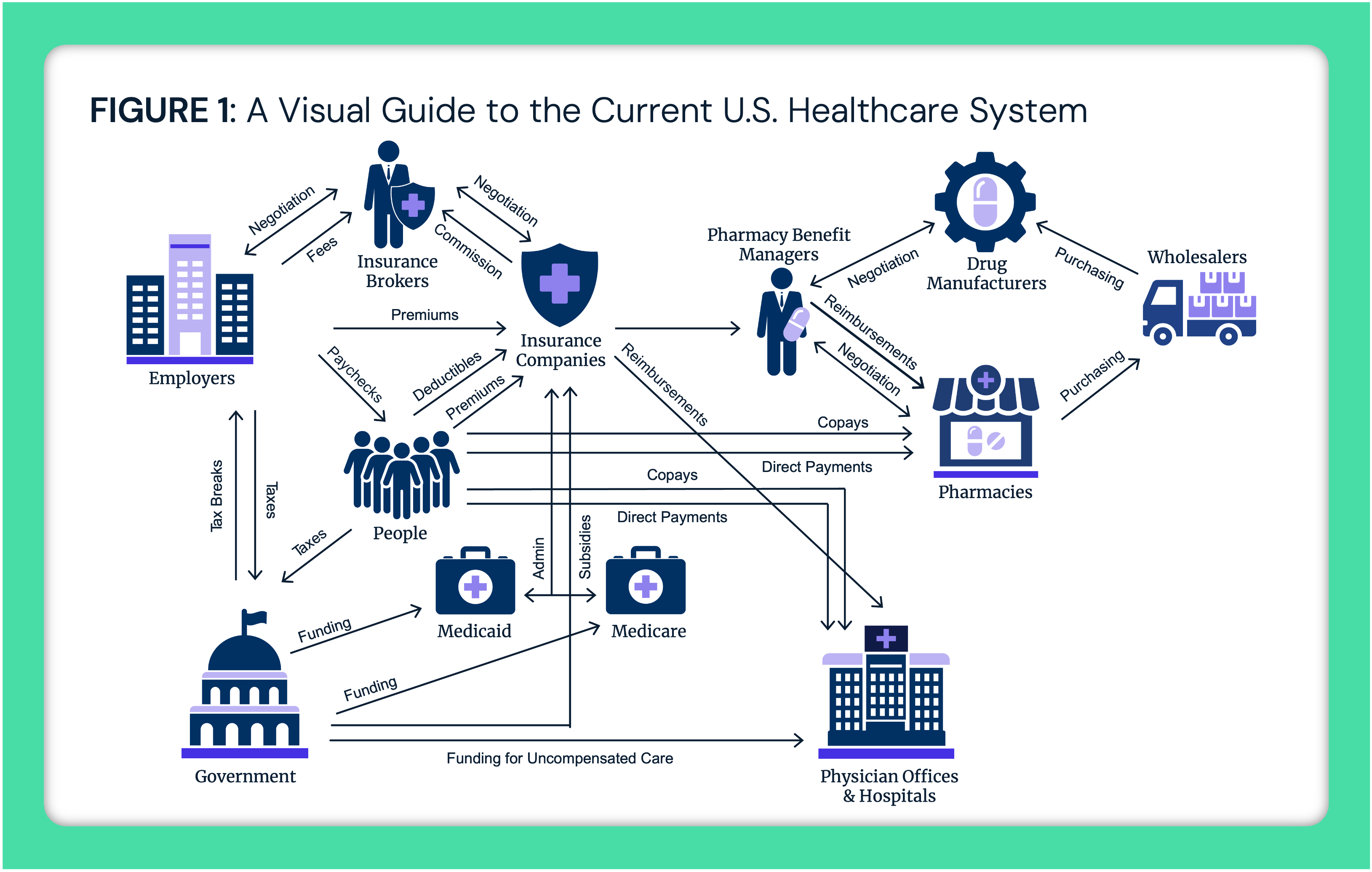
March 15, 2024, was "Match Day," the day U.S. medical students learned where they will train for medical residency. The results of Match Day present an opportunity to assess the healthcare workforce trainee pipeline. As provider shortages intensify due to burnout, early retirement and competition from new entrants, understanding both current workforce supply and future supply are critical to redress provider shortages.1 To gauge whether the physician trainee pipeline aligns with future supply needs, we examined the 2024 Resident Match results and compared these results to current workforce projections.
Background
During the 2024 Residency Match cycle, 50,413 MD and DO medical students registered, of which 44,853 certified a rank order of training preferences.2 Of applicants with certified rank ordered match lists, 80.2% matched to a first-year residency position. Compared to 2023, the total number of available residency positions increased by 2.8% (1,128 more positions).
Despite a record number of applicants and residency positions offered, the incumbent class of resident physicians is unlikely to address ongoing workforce shortages. The net number of physicians that started and stopped practicing between 2018 and 2022 resulted in a -2.3% workforce reduction.3 Seventy-four million Americans live in what the Health Resource and Services Administration (HRSA) designates as a "Primary Care Health Professional Shortage Area," and the American Medical Association estimates that by 2033, the nation will face a shortage of up to 124,000 physicians.4,5 In response, Federal, state and local governments are considering strategies to increase physician supply (e.g., funding career pathway programs and establishing grant programs to recruit or retain staff).6
Analytic Approach
We analyzed the results of the 2024 Main Residency Match, inclusive of PGY-1 and PGY-2 MD and DO applicants to quantify the number and percent of unfilled residency positions by specialty. Specialties with fewer than 70 available residency positions (e.g., nuclear medicine), transitional programs and preliminary programs were excluded from the analysis. We then analyzed HRSA's Workforce Adequacy Projections for 2023 to 2036, which apply an integrated microsimulation model to estimate current and future demand for and supply of healthcare workers to project the adequacy of provider supply by estimating new entrants to the workforce, worker attrition, population growth and demand for healthcare services.7
Findings
Family medicine had both the highest number (1,272) and percentage (6.5%) of unfilled residency positions among all specialties (Figure 1). Primary care specialties (i.e., family medicine, internal medicine and pediatrics) accounted for the majority of unfilled residency positions. Additionally, both emergency medicine (270 unfilled positions) and psychiatry (24 unfilled positions) did not fill all available positions. Conversely, specialist positions (e.g., vascular surgery, otolaryngology, thoracic surgery) saw match rates close to or at 100%.
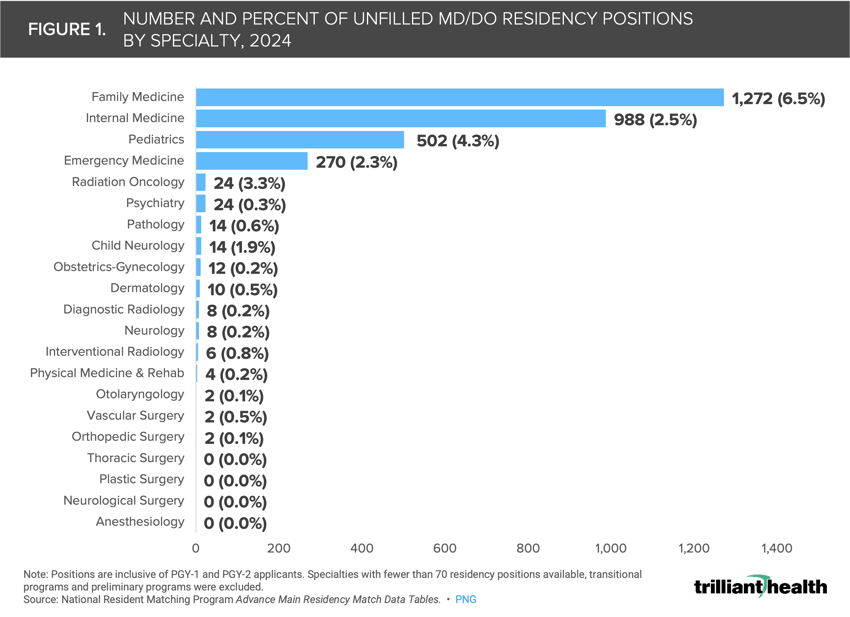
Notably, the four residency categories with the lowest fill rates are the physicians who serve as the gateway to the U.S. healthcare system for almost every American, since more than half of hospital admissions originate in the emergency department.8
Physician Supply Is Not Projected to Meet Primary Care Demand
While unfilled residency positions are an important indicator of physician supply, other factors such as burnout, early retirement and career switching also influence the adequacy of physicians. The extent of provider supply challenges within a market requires a market-level understanding of future demand for healthcare services.
Between 2023 and 2036, the national projected adequacy of most medical physicians is declining and below 100% (Figure 2). The specialties among the lowest projected adequacy rates for 2036 are internal medicine (75.8% adequate) and family medicine (78.3% adequate), while specialties with the highest adequacy rates are emergency medicine (122.9% adequate) and endocrinologists (109.6% adequate).
Despite the nearly 100% match rates for most surgical residency positions, the adequacy of most surgical specialties is declining and below 100% between 2023 and 2036 (Figure 3). Only colorectal surgeons are projected to meet demand by 2036 (100.3% adequate), while the projected adequacy for vascular surgeons is 64.3%.
In addition to examining which specialties are projected to be inadequate, we examined where physician adequacy rates are lowest. In 2023, primary care workforce shortage areas were concentrated in rural areas throughout the Midwest and Northwest, which trends are likely to persist given current projections.9 Across primary care physician specialties, adequacy projections are more positive in non-rural areas than rural areas (Figure 4).
The difference between adequacy for non-rural vs. rural varies by specialty, ranging from a difference of 5.8 percentage points (PP) for family medicine physicians (79.1% adequate in non-rural areas versus 73.3% adequate in rural areas) to 40.4 PP for geriatrics physicians (84.6% adequate in non-rural areas versus 44.2% adequate in rural areas).
Despite numerous initiatives to bolster the rural health workforce, current shortages and projected supply shortfalls suggest those efforts are falling short.10 Moreover, continued rural hospital closures threaten to exacerbate ongoing shortages in both the near and long-term by limiting the availability of rural residency programs.11
Conclusion
Access to healthcare services, particularly preventive services, is foundational to improve population health. What policies and initiatives will be effective to reengage the workforce and build a stronger culture for physicians, particularly those in rural areas? How can more medical students be encouraged to train in primary care specialties? To what extent are medical school debt and other financial concerns driving residents to choose higher-paying specialties?
Given the ongoing crisis facing the U.S. health system (e.g., increasing disintermediation of care, tepid demand for healthcare services, increasing acuity), record high medical residency applicants, program and position participation are positive indicators for a growing supply of physicians.12,13,14 However, growing supply will not alleviate ongoing shortages if growth is concentrated in adequately supplied specialties. Despite a record number of available primary care positions (19,423) that accounted for nearly half of all positions offered during the 2024 match cycle, the primary care fill rate fell from 2023 to 2024, suggesting that medical students are relatively uninterested in primary care. A persistently smaller pipeline for primary care physicians will undoubtedly exacerbate ongoing shortages and constrain adequacy levels for primary care physicians for years to come.
Moreover, these trends create a potential "doom loop" as a shrinking primary care workforce could contribute to growing dissatisfaction and distrust in the healthcare system, which, in turn, further suppresses demand as patients are discouraged by increasing difficulties in accessing primary care. While allied health professionals (e.g., nurse practitioners, physician assistants) already play a substantial role in primary care delivery and projected allied health supply is positive for offsetting gaps, the shortage of primary care providers persists.15,16 Similarly, many expected virtual care to extend capacity, but widespread access to telehealth has yet to move the needle. What new strategies are needed to bolster the primary care workforce? Are there community training programs that health economy stakeholders can stand up to engage individuals who already live in rural areas to pursue a career in medicine? To what extent have ill-considered, if well-meaning, regulatory and administrative burdens become a deterrent to becoming a physician or practicing until retirement? The health of American citizens will undoubtedly be impacted by the answers to these questions.
- Primary Care
- Social Determinants of Health
- Specialty Care
- Healthcare Workforce






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)




-2.png)
.png)