Research
Liver-Related Mortality and Healthcare Utilization Among Younger Men Is Growing
Jun 2, 2024 12:01:00 AMStudy Takeaways
- Mortality from liver disease and cirrhosis among ages 18-39 and 40-64 has generally increased since 2018, but the rate of change is higher in younger men. In parallel, utilization of health services for liver conditions in this age group has surged, with substantial geographic variability.
- Further examination of trends in select liver conditions for men ages 18-39 indicates different magnitudes of change by condition. Visits for alcoholic liver disease showed a substantial increase, increasing by 232.8% from 2018 to 2022.
- While increasing access to treatments that specifically address liver diseases is important, it will be more imperative for policymakers and other health economy stakeholders to address the primary risk factors that led to these conditions – notably excessive alcohol use and obesity.
The start of June marks National Men’s Health Month, an opportunity to raise awareness about health issues affecting men and boys and to encourage them to seek regular medical advice and early treatment for diseases and injuries.1 Liver disease is an emerging area of concern in men’s health, with increasing mortality attributed to liver disease and cirrhosis as a result of excessive alcohol use, worsening behavioral health status and decreasing primary care utilization. Therefore, research and investment in interventions to reverse this trend of growing liver-related disease burden is warranted.
Background
While the causes and risk factors for liver disease and cirrhosis (e.g., excessive alcohol use, obesity, chronic hepatitis) are well-documented, the disease burden for men under age 40 is less understood. Liver disease accounts for one in 25 deaths globally, posing a significant public health challenge.2 In terms of healthcare system financial impact, one study estimated five-year national hospitalization costs in patients with chronic liver disease reached $81.1B.3 Another study projects that from 2022 to 2040, costs associated with alcohol-associated liver disease alone will reach $880B, with $355B in direct healthcare costs and $525B in lost labor and economic consumption.4
Mortality from liver disease and cirrhosis among men ages 18-39 and 40-64 has generally increased since 2018, but the rate of change is higher in younger men. For men ages 18-39, mortality increased by 96.8% from 2018 to 2021 as compared to a 29.3% increase for men ages 40-64 during the same period (Figure 1).
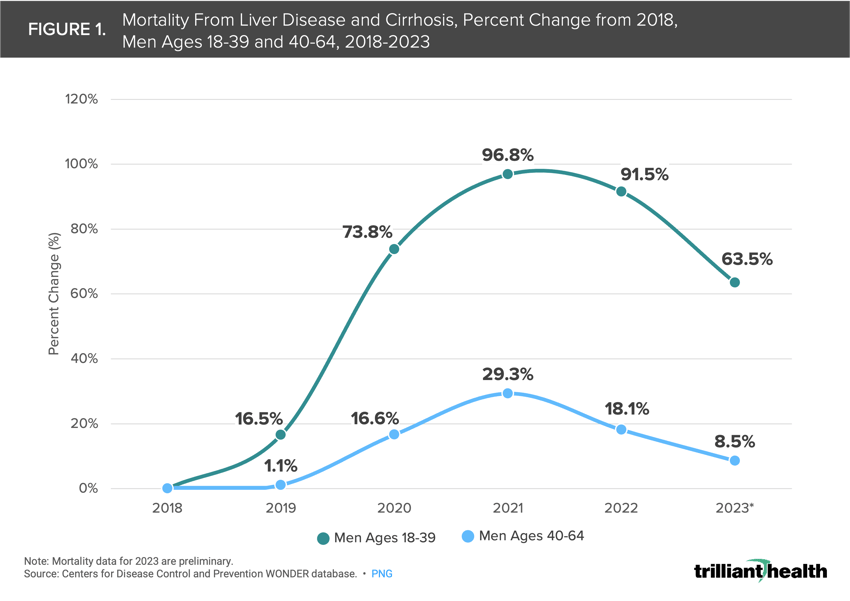
During the COVID-19 pandemic, deaths from excessive drinking among males increased approximately 27.0%.5 Notably in 2022, 10.5% of Americans ages 12 or older (29.5M individuals) had alcohol use disorder, including 16.4% of males ages 18 to 25.6 These trends are compounded by lower utilization of primary care and mental health services by men.7,8
Many liver conditions have limited pharmaceutical treatment options. Although emerging evidence suggests that GLP-1s – which are currently indicated for diabetes and weight loss – may offer treatment for liver disease, only three medications are approved to treat alcohol use disorder. Additionally, off-label use of gabapentin, an anti-seizure medication, shows signs of slowing the progression of alcohol-associated liver disease.9
Given these notable shifts in mortality due to liver disease in younger men in contrast to historic trends, we sought to analyze national and regional trends in select liver conditions.
Analytic Approach
We leveraged our national all-payer claims database to analyze utilization of health services attributed to select liver-related conditions for men ages 18-39 between 2018 and 2022. The CDC WONDER database was utilized to examine mortality from liver disease and cirrhosis among men ages 18-39 and 40-64 between 2018 and 2023. We examined patients with at least two medical visits since 2018 and analyzed the rate of health service utilization attributed to select liver-related conditions per 100K men ages 18-39, nationally and by state.
Findings
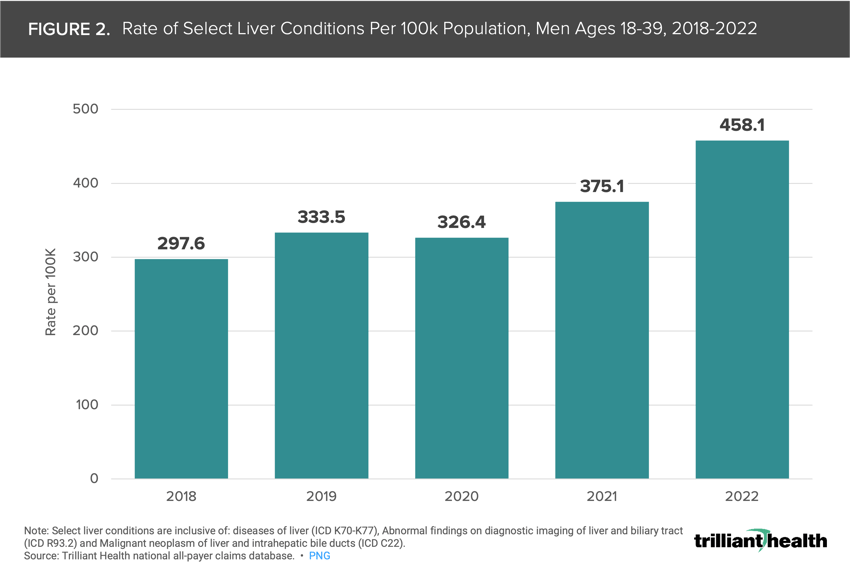
In parallel with growing mortality, the incidence rate of men ages 18-39 receiving care for select liver conditions per 100K population consistently increased, up 53.9% from 297.6 in 2018 to 458.1 in 2022 (Figure 2).
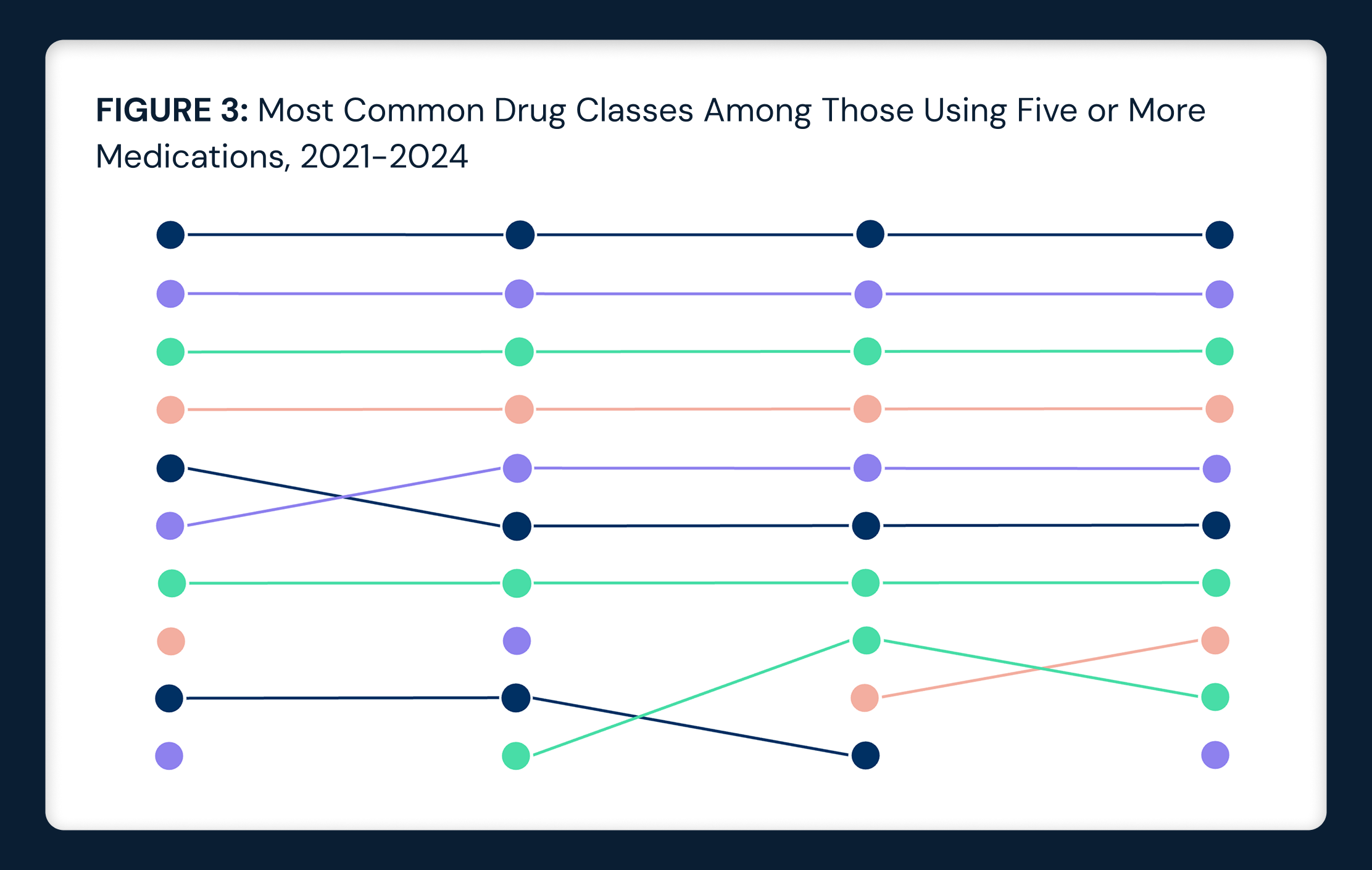
Further examination of trends in select liver conditions for men ages 18-39 indicates different magnitudes of change by condition. Visits for alcoholic liver disease showed a substantial increase of 232.8% from 2018 to 2022 (Figure 3). However, visits for chronic hepatitis decreased, declining by 17.1% in the same time period. Visits for fibrosis and cirrhosis of the liver (110.9%), hepatic failure (63.1%) and malignant neoplasms of the liver and intrahepatic bile ducts (54.6%) all increased.
Examining the rate of select liver conditions per 100K men ages 18-39 across states highlights wide geographic variability compared to the national rate of 458 per 100K in 2022. In 2022, California exhibited the highest rate (643 per 100K), closely followed by West Virginia (631 per 100K) and New York (626 per 100K) (Figure 4). Conversely, Idaho exhibited the lowest rate at 226 per 100K, with Wisconsin (283 per 100K) and Utah (287 per 100K) exhibiting lower-than-average rates. Thirteen states were above the national rate of 458 per 100K, while 38 states and D.C. were below the national rate. This variation suggests that regional factors, such as healthcare access, socioeconomic status, lifestyle and COVID-19 pandemic lockdown policies, may significantly influence the prevalence of liver conditions among men ages 18-39.

Conclusion
The rising trend of liver-related mortality and healthcare utilization among men ages 18-39 is alarming and a critical component in the declining health status of younger Americans.10 Our analysis reveals that mortality from liver disease and cirrhosis has surged dramatically in this age group since 2018, with a peak in 2021. The exacerbation of liver-related health issues among younger men can be attributed to several underlying factors. Behavioral health issues, such as increased stress, anxiety, depression and alcohol consumption attributed to Federal, state and local lockdown policies amid the COVID-19 pandemic, have significantly contributed to this trend. The reluctance of men to engage with primary care and mental health services further complicates efforts to address growing mortality and disease burden. Men are generally less likely to seek regular medical advice, which delays the diagnosis and treatment of liver conditions.
While recent findings suggest the potential efficacy of GLP-1s in improving liver function, existing treatments for common liver conditions remain limited. If GLP-1s are demonstrated to be efficacious, prioritizing access to affordable treatment in markets with high-prevalence populations could be a strategy to consider but it is likely to fall short. Putting aside the fact that GLP-1s are already in limited supply for the patients that need them, the marked variation in growth by the type of liver condition (as shown in Figure 3) is revealing. The substantial spike in alcoholic liver disease relative to all other types such as liver cancer and chronic hepatitis suggests lifestyle factors have played an outsized role relative to other risks. While increasing access to treatments that specifically address liver diseases is important, it will be more imperative for policymakers and other health economy stakeholders to address the primary risk factors that led to these conditions – notably excessive alcohol use and obesity. To what extent is increased alcohol use associated with the despair Americans experienced during the pandemic lockdowns? Did the “Zoom happy hour” tradition lead to more health consequences than social connectedness? Did these behaviors of older adults during this time of stress and isolation normalize unhealthy habits for younger adults? What are the longer-term term effects of more youth struggling with excessive alcohol use as they age? To what extent will this trend of excess morbidity and mortality in younger men exacerbate the already troubling trends in fertility? How does the convergence of this liver disease trend in younger men with other findings we have previously noted in younger adults (e.g., myocarditis, oncology) play out?
All health economy stakeholders must consider the drivers and societal consequences of increasing incidence of, and mortality attributed to, liver disease in younger men and what these trends signal for the future public health and economic burden plaguing the U.S. health economy.
Thanks to Colin Macon and Katie Patton for their research support.
- Social Determinants of Health
- Specialty Care
- Life Sciences
- Disease Burden






















.png)

















.png?width=171&height=239&name=2025%20Trends%20Report%20Nav%20(1).png)