The Compass
Sanjula Jain, Ph.D. | July 21, 2024Patient Volumes for Digestive Cancers Are Up for Younger Age Groups, Jeopardizing Improvements in Mortality
You are currently viewing the public version of Studies. To unlock the full study and additional resources, upgrade your subscription to Compass+.
Last week, we examined emerging trends in patient volumes for the most common cancers in the U.S. through 2023.1 We found that while overall colon cancer patient volumes were lower in 2023 compared to 2018, volumes increased among patients younger than 45. These initial findings, combined with indicators of growing early-onset colon cancer, prompted further investigation into the factors influencing colon cancer mortality, incidence and prevalence.
Background
Colon cancer is the third most frequently diagnosed cancer and the second leading cause of cancer-related deaths overall. It is the primary cause of cancer death in men under 50. More than 50% of colon cancer cases and deaths are linked to lifestyle risk factors such as smoking, unhealthy diet, excessive alcohol consumption, physical inactivity and obesity.2 The U.S. Preventive Services Task Force recommends colon cancer screening for adults ages 45 to 75.3
Although media reports have highlighted “anecdata” signaling an increase in colon cancer among younger adults, our prior research found that colon cancer patients treated in 2022 were generally healthier than those treated in 2017, as evidenced by a 13.9% lower average risk adjustment factor (RAF) score.4
After meaningful improvements in overall colon cancer incidence and mortality over time, a recent reversal of this trend, particularly in younger patients, has significant implications for the overall health status of the U.S. population and healthcare spending. Therefore, we examined trends in mortality, incidence, screening and prevalence of colon cancer, along with other digestive cancers.
Analytic Approach
We first used data from the National Cancer Institute and the Center for Disease Control and Prevention’s (CDC) WONDER database to examine colon cancer incidence and mortality. Next, we analyzed cancer screening utilization rates and patient volumes for colon cancer and other digestive cancers – rectum, pancreas, stomach, liver and unspecified sites – from 2018 to 2023 leveraging our national all-payer claims database. Data was analyzed for the entire patient population and two age groups: 0-45 and 46 and older.
Findings
According to the CDC's WONDER database, the crude mortality rate for colon cancer in 2023 was 14.9 per 100K, slightly up from 14.7 per 100K in 2019. However, changes in mortality vary by age. For women ages 45 to 54, the mortality rate increased by 0.7 per 100K, while for men in the same age group, it increased by 0.3 per 100K (Figure 1). For men ages 55 to 64, the rate increased by 0.8 per 100K, but for women in this age group, it declined by 0.1 per 100K. The mortality rate increases for both men and women ages 25 to 34 and 35 to 44 ranged from 0.1 to 0.3 per 100K. Notably, while the mortality rate declined by 10.3 per 100K for women ages 85+, it increased by 3.8 per 100K for men ages 85+, despite declines for men and women ages 75 to 84.
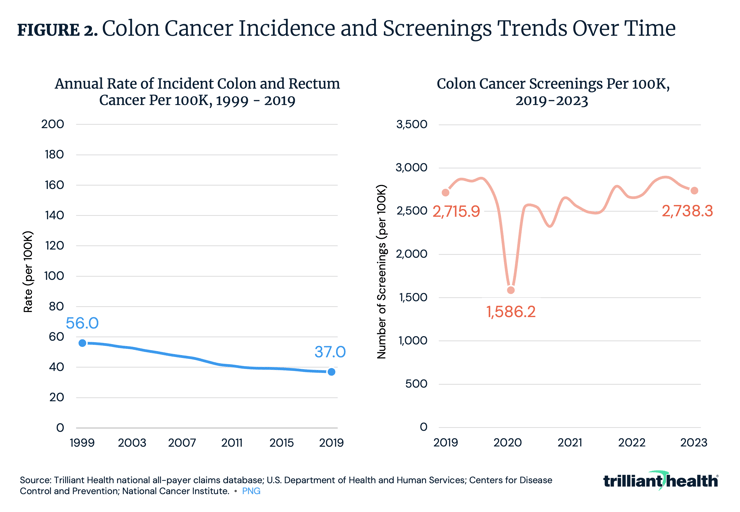
From 1999 to 2019, colon cancer incidence declined by 33.9%, decreasing from 56 to 37 cases per 100K (Figure 2). However, the COVID-19 pandemic disrupted cancer screening and diagnosis. Screening levels trended below 2019 averages from 2020 to 2022 but returned to pre-pandemic levels as of 2023.
Aggregate patient volumes for colon cancer decreased by 5.0% from Q4 2018 to Q4 2023 (Figure 3). However, when segmenting patients by age, notable differences emerge. For patients ages 46 and older, volumes decreased by 5.6%, while for those ages 45 and younger, volumes increased by 10.0%, aligning with emerging reports of a rise in colon cancer among younger Americans. After two decades of consistent declining incidence through 2019, the disruptions to care and impacts from COVID-19 on screening, disease progression and diagnosis impacted the number of people being diagnosed and treated for colon cancer.
Thanks to Colin Macon and Katie Patton for their research support.
- Specialty Care
- Disease Burden
You are currently viewing a free preview of our premium studies. To receive new studies weekly, upgrade to Compass+ Professional.
Sign UpSee more with Compass+
You are currently viewing the free version of this study. To access the full study, subscribe to Compass+ Professional for $199 per year.
Sign Up for Compass+

